May is Lupus Awareness Month
Put on Purple & Test – Don’t Guess! (for Lupus Awareness)
May’s Lupus Awareness Month is a call to attention for lupus awareness and its impact on the lives of millions of individuals and families living with lupus. Put On Purple Day is held May 17th – wear purple and tell people why you are showing your support of lupus!
Lupus is a chronic autoimmune condition that causes the immune system to attack the body’s own tissues and organs, including joints, kidneys, liver, lungs, heart, brain, blood, and skin. Building awareness of lupus is essential to improve early diagnosis and treatment, and ensure that people with lupus are aware of the support and resources available to help them manage the disease.
Childhood lupus accounts for 10-20 percent of all people with lupus. A study on childhood lupus quality of life found children and adolescents have daily symptoms that limit function, mood, and learning, cause worry about the future, and impact personal and family relationships. The researchers concluded that psychosocial support, health education, and personalized treatment plans are necessary to improve quality of life in childhood lupus.
Diagnosing Lupus: Take A Vibrant Wellness Approach
The time from onset of symptoms to diagnosis of lupus is long, and symptoms often progress faster than current diagnostic tests can detect early stages of disease; meanwhile, people’s health and quality of life suffer. Diagnosing lupus is difficult because signs and symptoms vary considerably from person to person and overlap with those of many other disorders. No one test can diagnose lupus. A combination of physical examination, signs and symptoms, imaging tests, and laboratory tests leads to the diagnosis.
Laboratory tests for lupus include:
- Complete blood cell count (CBC): Low red blood cells, low white blood cells, and low platelet count commonly occur in lupus, however may occur in other conditions as well.
- Erythrocyte sedimentation rate (ESR): A high sedimentation rate may indicate a systemic disease, such as lupus, however this test isn’t specific for any one disease. It may be high if you have lupus, an infection, another inflammatory condition, or cancer.
- Kidney and liver function tests: Lupus can affect kidney and liver function. These tests are not specific to lupus only.
- Urinalysis: If lupus has affected the kidneys, which occurs in later disease stages, urinalysis may show increased protein or red blood cells in urine.
- C–reactive protein (CRP): The CRP test measures inflammation in the body, which can be high in lupus. This test is not specific to lupus only.
- Antinuclear antibody test (ANA): The presence of ANA antibodies has long been considered a ‘gold standard’ leading to a diagnosis of lupus as 95% of people with lupus test positive for ANA, however, there are limitations to this test as a number of other non-lupus causes can trigger a positive ANA, including infectious and other autoimmune diseases.
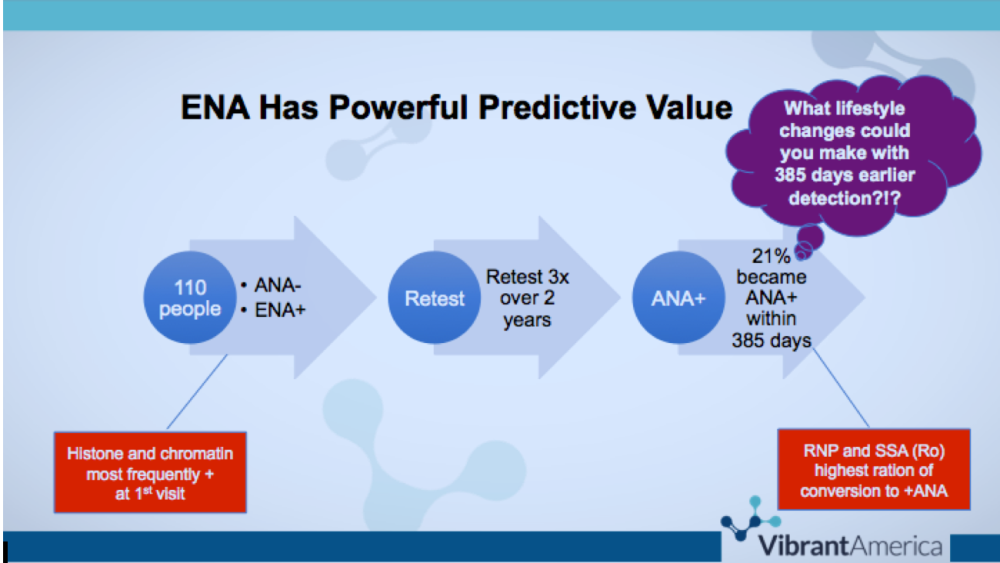
- Extractable nuclear antigens test (ENAs): The presence of ENA antibodies (Jo-1, Scl-70, Sm, RNP, SSA (Ro), SSB (La), chromatin, centromere, histone, and RNA polymerase III) may exist years earlier than ANA antibodies, and may help early detection of lupus.
*Preventive Health Tip- think of ANA and ENA antibodies as powerful predictors of disease- it’s better to predict disease early rather than test for/diagnose advanced disease!
The Vibrant Wellness Connective Tissue Disorders® test with simultaneous testing of ANA and ENA antibodies is the most comprehensive test in the industry for early detection of connective tissue disorders, including lupus!
A Vibrant America study followed 110 people who were negative for ANA antibodies but who were positive for ENA antibodies. When retested three times over two years, twenty-one percent of people became positive for ANA within 385 days. What lifestyle changes could you make with 385 days earlier detection????
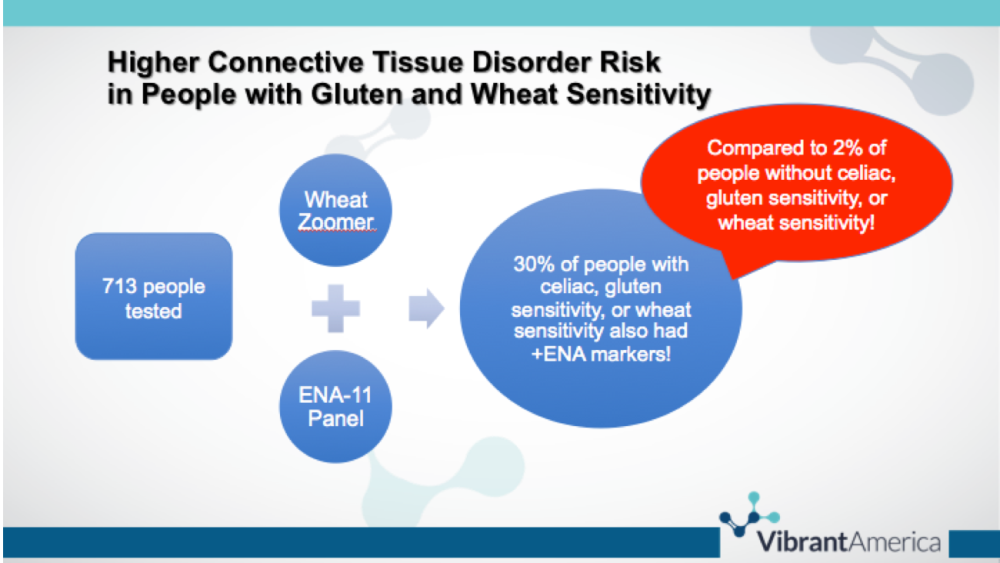
 But wait, there’s more!! People with connective tissues disorders, including lupus, are at higher risk of gluten and wheat sensitivity…
But wait, there’s more!! People with connective tissues disorders, including lupus, are at higher risk of gluten and wheat sensitivity…
A Vibrant America study tested 713 people with a Vibrant Wheat Zoomer and Vibrant Connective Tissue Disorder panel. Thirty percent of people with a positive celiac panel, gluten sensitivity, or wheat sensitivity also had positive ENA markers! This explains why many people with lupus report improved health-related quality of life on a gluten-free diet!
Managing Lupus: Take a Lifestyle Medicine Approach
- Diet: One study of diet therapy found 22% of people with lupus found their symptoms and mood improved as a result of diet therapy. Diet therapies to consider include elimination diet (eliminating gluten and other food antigens that mimic human antigens in autoimmune disease; elimination diets should be based on food sensitivity testing), anti-inflammatory diet, Paleo-autoimmune diet, and vegan diet. Consult with an integrative and functional medicine provider to find out which diet therapy is best for you.
- Fitness: Here’s why exercise is helpful for managing lupus…
- Exercise strengthens body systems affected by lupus
- Exercise reduces inflammation
- Exercise helps control weight gain which can contribute to and worsen lupus flare-ups
- Exercise and movement can decrease muscle stiffness and increase range of motion
- Exercise uplifts mood, making it easier to cope with stress, and can reduce fatigue
- Sleep Support: Sleep disorders occur in more than half of people with lupus and are associated with high disease activity- the worse you sleep, the worse your lupus, the worse you feel! Stick to a sleep schedule of the same bedtime and wake time, try a relaxing bedtime ritual (and avoid stressful activities before bed), sleep in a room temperature between 60—67 degrees (for kids it’s 65-70 degrees), avoid bright light in the evenings, and get sunlight in the morning. For more information, check out the National Sleep Foundation online sleep tools and tips, and try an app like SleepCycle® to track sleep quality and trends.
- Stress Management: People with high stress and post-traumatic stress disorder (PTSD) are more likely to develop autoimmune disease. Stress management may help prevent, delay onset, slow progression of, better manage, or reverse autoimmune disease.
- Social Support: Group psychotherapy, cognitive behavioral therapy, and mindfulness studies have shown promising results for improvement in fatigue, depression, pain and quality of life for people with lupus. Social support of spouses, family, and friends helps coping, resilience, and quality of life in people with autoimmune disease.
References
- Fangtham, M., et al. “Non-Pharmacologic Therapies for Systemic Lupus Erythematosus.”Lupus, Apr. 2019, doi:1177/0961203319841435.
- Harry, O., et al. “Self-Management and Adherence in Childhood-Onset Systemic Lupus Erythematosus: What Are We Missing?”Lupus, Mar. 2019, doi:1177/0961203319839478.
- Robinson, G. A., et al. “Diet and Lupus: What Do the Patients Think?”Lupus, Apr. 2019, doi:1177/0961203319845473.
- National Sleep Foundation. Healthy Sleep Tips. https://www.sleepfoundation.org/articles/healthy-sleep-tips Accessed May 7, 2019.
- Song H, Fang F, Tomasson G, et al. Association of Stress-Related Disorders With Subsequent Autoimmune Disease. 2018;319(23):2388–2400. doi:10.1001/jama.2018.7028
- Carpenter, Delesha M et al. “The Relationship Between Social Support, Social Constraint, and Psychological Adjustment for Patients with Rare Autoimmune Disease.” Current Rheumatology Reviews 12,3 (2016): 232-238.
- Vibrant America. White Paper: Vibrant America ANA ENA panel for connective tissue disorder. https://www.vibrant-america.com/wp-content/uploads/2018/06/MC-0025-00-CTD-White-Paper.pdf Accessed May 7, 2019.
Vibrant Wellness. White Paper: Vibrant Wellness Wheat Zoomer-ENA overlap. https://www.vibrant-america.com/wp-content/uploads/2018/06/MC-0046-01-Wheat-Zoomer-ENA-White-Paper.pdf Accessed May 2019