Don’t judge a book by its cover: Are harmful bacteria masquerading as “good guys” in your gut?
You might have read the bottle of your new probiotic wondering what exactly all these different bugs do and if you really need them?
In the 1980’s and 90’s people began to hear about how Lactobacillus acidophilus can help with a yeast/candida problem or how it helps to take probiotics after a course of antibiotics.
Fast forward to 2019 and what we still know is only a grain of sand compared to the vast empire known as our microbiome.
Within that vast empire lie a complex synergy, energetics, community, and division of labor. All processes created and maintained to benefit the host – you.
Thus, when we take a snapshot with the latest and greatest stool testing methodology, we may have a look of wonder on our faces when looking at the results.
What are all these bacteria? What do they mean? Is it good? Is it bad? More importantly….what do I really need to know?
The Vibrant Advantage
The most important thing to remember when looking at your stool test is that we can often identify patterns of imbalance.
Fortunately, we have reached the level of knowledge about bacteria that allows us to identify whether a lack of beneficial flora, commensal flora, or diversity can put us at risk for certain diseases and which ones.
Also, we can see patterns of excess – such as too many bacteria that thrive due to the overuse of antibiotics (which can happen after just one course! [1]), as well as ratios that display excesses and primary imbalances -which we know can fuel inflammation.
Gastrointestinal inflammation can give rise to irritable bowel syndrome, heartburn, ulcers and inflammatory bowel disease. It is nothing to sneeze at, but rather a call to action. Taking notice of these patterns gives us an extraordinary view into a world that is still virtually unknown.
For example, look at this snapshot of a stool test done by one of our Vibrant patients with the previous version of our Gut Zoomer test:
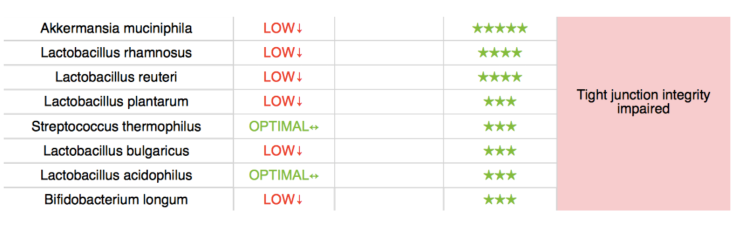
Here we see an example of low commensal bacteria – many of which are known to be beneficial and to play significant roles such as defense against opportunistic pathogens as well as mitigating inflammatory damage from pathogens.
These types of symbiotic bacteria are also known to maintain the mucosal layer in the gut, enhance motility, and protect your immune system, in addition to a myriad of other functions (1).
These bacteria can be adversely affected by the use of antibiotics, medications (such as proton pump inhibitors, oral contraceptive agents, Advil or other NSAID’s), stress, alcohol, nutritional deficiency, poor diet (excess sugar and processed foods), pathogen excess and toxicity (eg from heavy metals, chemicals, etc).
For this particular patient, determining the origins of her low levels of beneficial bacteria was not obvious, however she had several courses of antibiotics a decade prior to the test.
Thus adopting good detective skills in assessing the true nature of her or anyone’s dysbiosis becomes foundational to creating an effective treatment plan.
In this scenario, symptoms of very low beneficial bacteria can resemble the same symptoms you might experience if you had too many harmful bacteria – and testing would be the only way to know which situation you have.
When Good Bacteria Go Bad
Another well-known side effect of using antibiotics is the unwitting promotion of commensals that become unfriendly or resistant.
This is demonstrated in the case of SIBO (Small Intestinal Bacterial Overgrowth), for which Vibrant’s researchers have identified clear patterns pointing to (although not diagnosing) SIBO.
Such a pattern can be seen here on Vibrant’s updated Gut Zoomer.
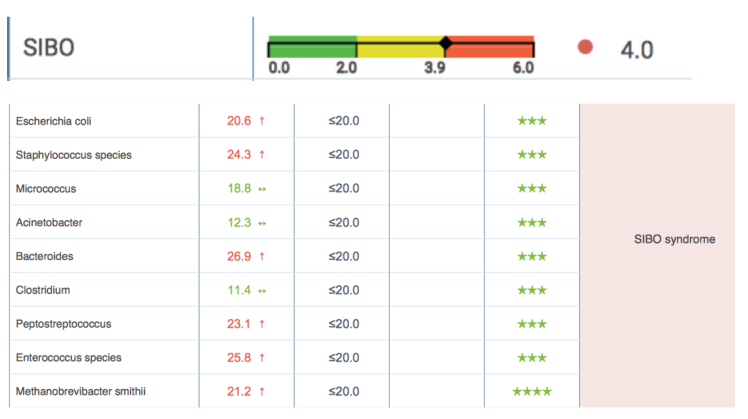
Commensal bacteria such as E. Coli, Streptococcus, Enterococcus and Staphylococcus can become less friendly under physiologic conditions (exposure to antibiotics, glyphosate, foodborne illness, etc) and can influence changes in motility/digestion that manifest in digestive symptoms.
Like anything else in chronic conditions, the goal is to support the patient’s constitution, reduce their susceptibility to experiencing uncomfortable symptoms, and to choose safe foods that they are not reacting to.
Diet is Still Important
Food does play a major role in either laying the foundations for inflammation or promoting the growth of beneficial bacteria that can offset imbalance induced by the use of antibiotics.
Patients can also benefit greatly when their provider orders a bundle of Vibrant Food Zoomers with their Gut Zoomer to accurately assess which foods may be causing unwanted, negative immune responses in their body.
Using Vibrant’s Gut Zoomer testing technology allows practitioners to gain insight to patterns of commensal bacteria growth, which may be causing current symptoms or those that could predictably cause suffering in the future, and provides an invaluable snapshot of homeostasis or dysbiosis in the microbiome.
References
1) Bhaskaran N, Quigley C, Paw C, Butala S, Schneider E, Pandiyan P. Role of Short Chain Fatty Acids in Controlling Tregs and Immunopathology During Mucosal Infection. Frontiers in Microbiology, 2018; 9 DOI: 10.3389/fmicb.2018.01995
2) Round, JL Marzmanian SK. The Gut Microbiota Shapes Intestinal Immune Responses during Health and Disease. Nat Rev Immunol. 2009 May;9(5):313-23. doi: 10.1038/nri2515