The Surprising Impact of Stress on Gut Health
Our body’s response to stress is unique in that it can manifest both mentally and physically. You're likely familiar with phrases such as “sick to my stomach,” “my stomach is in knots,” and “gut- wrenching.”
But did you know that these adages connecting stress, the gut, and mental and physical health are actually backed by science?
This interconnectivity is thanks to the sophisticated communication network between the gut and the brain, known as the gut-brain axis.
In this article, we’ll dig deeper into the gut-brain axis and learn how stress impacts mental and physical health through this communication network. Plus, we’ll discuss precision testing and nutrition and lifestyle strategies to address gut inflammation and promote healing.
The Gut-Brain Axis
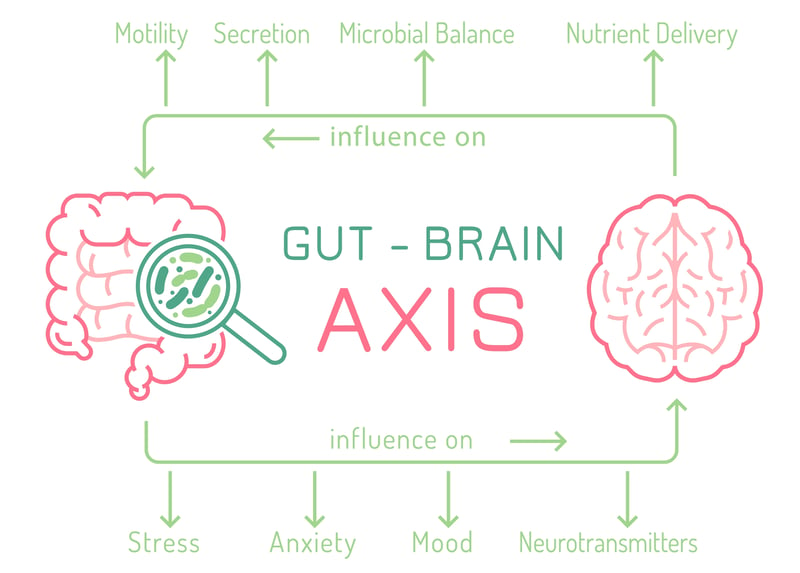
The gut-brain axis is a complex network of nerves that allows the gut and central nervous system to communicate, linking the brain's emotional and cognitive regions with gut function.
This highway of nerves explains why digestive disorders like irritable bowel syndrome (IBS) often accompany mood disorders.
The gut-brain communication network maintains the gastrointestinal functions that support behavior and bodily processes, and also allows feedback from the gut, which influences mood, behavior, and brain function.
There are various mechanisms involved in the gut-brain axis, including:
- Afferent and efferent neural projection pathways
- Bidirectional neuroendocrine signaling
- Immune activation and signaling from gut to brain
- Modulation of enteric sensory-motor reflexes
- Enteroendocrine signaling
Stress can impact the gut-brain axis by affecting gut microbiota, a key player in regulating the various pathways of this communication network.
Gut bacteria play an essential role in the gut-brain axis by interacting locally with intestinal cells and the enteric nervous system (ENS) and directly influencing neuroendocrine and metabolic systems.
The alteration of gut microbiota in experiments has been shown to influence stress responsiveness, anxiety-like behavior, and the set point for activation of the neuroendocrine hypothalamic-pituitary-adrenal (HPA) stress axis.
How Stress Impacts the Gut
Environmental factors and behaviors affect gut microbiome diversity even more than genetics.
Stress, along with mood and diet, are key factors that can significantly influence which gut microbes thrive.
Stress can impact gut health by disturbing the balance of gut bacteria. Stress and depression cause heightened inflammation in the body, which stimulates the production of pathogenic bacteria that can lead to dysbiosis (imbalanced gut bacteria) and leaky gut.
Both chronic and acute stress can disturb microbiota balance within the inside of the gut (lumen) and the border (mucosal lining).
Even short-term exposure to stress can impact the gut microbiome by altering levels of the main groups of bacteria.
Animal studies show that stress can rapidly impact gut bacteria balance. Additionally, one in vitro study revealed that catecholamines (stress hormones) can increase levels of specific harmful bacteria by 10,000-fold and amplify their infectiousness in 14 hours.
These pathogens can overpopulate the gut, decreasing the prevalence of beneficial, immune-boosting bacteria. This imbalance can cause leaky gut and leave patients more susceptible to conditions like autoimmune disease and infection.
The Vicious Cycle of Stress, Gut Health, & Mental Health

Due to the gut-brain connection, stress and mood disorders often accompany one another. Studies have found differences in gut bacteria composition and function in those with major depressive disorder compared to non-depressed individuals.
Some data link the dominance of harmful gut bacteria to depression. When comparing depressed with non-depressed individuals, researchers found 279 different bacteria-synthesized proteins among those with depression, primarily related to glucose and amino acid metabolism—processes that may be associated with inflammation.
Not only does stress impact microbiota balance in the gut, but it can also increase intestinal permeability, which leads to leaky gut. One responsible party for this is the stress hormone cortisol, produced as a part of the stress response. Cortisol can weaken gut barrier function, leading to a state of leaky gut.
Stress, diet, and other lifestyle factors all play a role in gut dysbiosis, which causes intestinal permeability. Gut dysbiosis itself can also impact health habits like diet. These physical and behavioral changes can further disrupt stress response systems like the immune, endocrine, and nervous systems, triggering a domino effect of chronic stress and mental health disorders like depression.
Assessing Gut Health Using Precision Testing
With so many factors influencing gut health, it’s necessary to take a holistic view of health by assessing patient history, lifestyle, diet, gut health, and potential inflammatory triggers.
The Vibrant Wellness Gut Zoomer can reveal critical data on gut health, allowing you to assess bacteria, yeast, viruses, and parasites in the gut microbiome alongside relevant digestive and inflammatory markers.
The panel tests for over 170 species of bacteria, 67 different pathogenic microorganisms, functional markers of digestion and inflammation, and the entirety of DNA from all microorganisms tested.
This can reveal any infections or overgrowth of specific bacteria that can contribute to both gastrointestinal and neurological symptoms.
Markers include pathogenic fungi such as Candida albicans, an opportunistic fungal yeast species that can overgrow when the gut is in a state of dysbiosis, chronic infection, or immune dysregulation, all of which can be triggered by stress.
The Gut Zoomer also tests for beneficial bacterium like Akkermansia and Bacteroides, which are linked to the stress response.
Animal studies have shown reduced levels of both of these bacteria when the body is exposed to stress and infection. Thus, testing for levels of various beneficial bacteria helps determine if stress is a cause of dysbiosis and gut inflammation.
The panel also detects inflammatory markers such as calprotectin (a protein found in white blood cells) and fecal lactoferrin (glycoprotein) to help determine if the gut is in an inflammatory state, which stress can trigger.
The 5-R Gut Health Protocol
.png?width=800&height=500&name=Antioxidant%20(10).png)
Once gut health is assessed with testing and patient evaluation, you can help patients heal chronic inflammation with the 5-R Protocol. This five-step framework supports and restores the balance of the gastrointestinal system by:
1. Removing known gut irritants and “triggers,” including known food sensitivities, allergies, and intolerant foods. Be aware that food sensitivities or allergies may be “hidden” or “undetected.”- If Small Intestinal Bacterial Overgrowth (SIBO) is suspected, consider avoiding high FODMAP foods (foods high in fermentable carbs).
- Also, remember that personalizing the food plan to remove other potential triggers, such as lectins, histamines, salicylates, grains, and others, is essential.
2. Replacing or finding alternatives for digestive support (if applicable). Consider including bitters and apple cider vinegar in the patient’s diet to help digestion alone.
3. Reinoculating the gut with prebiotic and probiotic-rich foods and a diverse diet to improve the diversity of the microbiome.
4. Repairing the gut lining and any gut damage, such as inflammation or immune system damage.
5. Rebalancing the nervous system and the gut by focusing on healthy lifestyle interventions such as stress management, sleep, and more.
For nutrition recommendations, access the complete Gut Health Food Plan.
Additional Strategies to Support Gut Health
Now that we've discussed the role of a balanced diet in promoting gut health, let's explore some additional strategies. While nutrition is undeniably important, there are many other ways to further enhance gut health and reduce chronic inflammation.
Additional strategies to support gut health and reduce chronic inflammation include:
- Supplementation, including omega-3 fatty acids, probiotics, prebiotics, curcumin, and L-Glutamine
- Physical activity, including aerobic exercise, yoga, and resistance training
- Stress management techniques, including meditation, cognitive-behavioral therapy, deep breathing, and adequate sleep
Monitoring Patient Progress: The Key to Longterm Gut Health

One of the crucial components of managing and improving gut health, particularly under the influence of stress, is diligent monitoring of the patient's progress. This is an important step as it allows you to not just identify issues, but also to measure improvements over time and alter treatment plans to better fit an individual's evolving needs.
Re-testing at regular intervals using functional tests like the Gut Zoomer, provides critical insights into the current state of a patient’s gut health. This tool delves into various markers related to digestion, absorption, inflammation, immune function, and the gut microbiome to help you not only measure improvements over time but also identify new or overlooked issues.
One 2021 study found that the amount of microbiota found in daily samples can vary up to 10 times from one sample to another. Over a longer period, like six weeks, this difference can be even more drastic—up to 100 times. Additionally, other signs show that these changes or differences happen over time, which is called temporal variability.
As gut health is dynamic and influenced by various factors, including diet, sleep, exercise, and stress, tracking a patient's progress enables tailored adjustments to their treatment plans. These modifications can encompass changes in medication, dietary recommendations, and stress management techniques, and are essential due to the individual variability in treatment response.
The connection between the gut and mind through the gut-brain axis allows both somatic systems to influence one another. This means that psychological processes like the stress response can impact your physical gut health—and vice versa.
Regular precision testing and re-testing, along with nutrition and lifestyle strategies, allows you to use the body’s natural communication highway between the gut and brain to gain information on gastrointestinal health while illuminating neurological symptoms like anxiety and depression.
Armed with this knowledge, you can get to the root of both intestinal and neurological symptoms and create holistic, individualized treatment plans to promote healing.
Regulatory Statement:
The general wellness test intended uses relate to sustaining or offering general improvement to functions associated with a general state of health while making reference to diseases or conditions. This test has been laboratory developed and its performance characteristics determined by Vibrant America LLC and Vibrant Genomics, a CLIA-certified and CAP-accredited laboratory performing the test. The lab tests referenced have not been cleared or approved by the U.S. Food and Drug Administration (FDA). Although FDA does not currently clear or approve laboratory-developed tests in the U.S., certification of the laboratory is required under CLIA to ensure the quality and validity of the tests.
 By
By