Gut Microbiome and Hormonal Balance: Key Clinical Insights for Practitioners
Understanding the connection between the gut microbiome and hormones is vital for maintaining your patients’ hormone balance. The gut-hormone axis plays a key role in regulating various endocrine functions, impacting conditions such as PMS, menopause, adrenal dysfunction, and fertility issues. Mastering this relationship allows you to develop comprehensive and personalized treatment plans for patients with hormonal imbalances.
Combining gut microbiome analysis with advanced hormone testing gives a precise picture of how hormones are produced, metabolized, and excreted. Explore the critical roles of the gut microbiome's impact on vital hormone regulation, while highlighting evidence-based strategies that you can initiate in your practice immediately.
Table of Contents
The Relationship Between the Gut Microbiome and Hormonal Health
Estrogen and the Estrobolome
One of the most significant interactions between the gut and hormones occurs through estrogen metabolism. The estrobolome is a subset of gut bacteria comprised of Escherichia coli, Enterobacteriaceae, Bacteroidetes, Firmicutes, Proteobacteria, and Actinobacteria. These strains modulate estrogen levels by producing beta-glucuronidase, an enzyme that influences estrogen reabsorption.1
An imbalance of these microorganisms (dysbiosis) in the gut can lead to excessive or insufficient estrogen circulation. This contributes to hormonal symptoms such as PMS, fibroids, endometriosis, and menopausal complaints.1
Improper estrogen metabolism can also lead to an accumulation of harmful estrogen metabolites. This increases the risk of estrogen-dominant conditions, including breast and ovarian cancer.2 Optimizing gut health is thus crucial for maintaining balanced estrogen levels.
Estrogen influences the composition of the gut microbiome diversity and also significantly impacts the gastrointestinal (GI) system as a whole. Fluctuations in estrogen levels affect overall gut health, particularly during menstruation and menopause.3
Too much of this hormone can reduce gut motility, leading to constipation, while lower estrogen levels may cause increased motility or diarrhea. Estrogen also supports the intestinal lining by promoting mucus production and maintaining tight junctions between epithelial cells, preventing leaky gut and inflammation.4
Cortisol Regulation and the Gut-HPA Axis

The hypothalamic-pituitary-adrenal (HPA) axis, which governs stress responses, is closely linked to the gut microbiome. Gut dysbiosis has been shown to heighten inflammatory cytokines, disrupting HPA axis function and leading to dysregulated cortisol levels.5 An imbalance in cortisol can contribute to fatigue, weight gain, mood disorders, and metabolic dysfunction.5
Increases in cortisol levels affect the gut microbiota by altering gut transit time, intestinal permeability, and nutrient availability. This can, in turn, impact the composition and diversity of the microbiota.6,7 Additionally, increases in cortisol can lead to abnormalities in other sex hormones.8
Research suggests that gut bacteria influence cortisol secretion through direct signaling pathways, affecting adrenal output and stress resilience.5 Addressing microbial imbalances can help regulate cortisol production and mitigate stress-related conditions.
Progesterone, Inflammation, and the Microbiome

Progesterone is a critical hormone for reproductive health. Its levels can be influenced by intestinal inflammation and microbiome diversity. Chronic gut inflammation elevates lipopolysaccharides (LPS), which trigger immune responses that lower progesterone.1 This can contribute to irregular cycles, implantation failure, and infertility.
Progesterone promotes the growth of bifidobacterium species, an effect that is increasingly noticeable during the later stages of pregnancy.9 Gut bacteria additionally act to convert progesterone to neurosteroids such as allopregnanolone, which affects the brain and nervous system. Low levels of allopregnanolone can contribute to postpartum depression and mood and psychiatric disorders.10
A well-balanced gut microbiome supports optimal nutrient absorption, reducing inflammatory responses and promoting hormonal stability. Restoring gut health can be an essential step in improving progesterone levels and reproductive function.
Testosterone and Gut Health
Testosterone is essential for muscle growth, metabolic function, mood regulation, and libido in both men and women. Emerging research suggests that gut microbiota significantly impact testosterone levels through multiple mechanisms, including inflammation regulation and nutrient absorption.11,12,13 Dysbiosis and chronic gut inflammation can lead to increased oxidative stress, which negatively impacts testosterone synthesis.
Elevated levels of testosterone in males and females were shown to correlate to a more diverse microbiota and quantity. Specifically, those with elevated levels of testosterone demonstrated higher quantities of Acinetobacter, Dorea, Ruminococcus, and Megamonas.14
Certain bacterial strains, such as Akkermansia muciniphila, have been associated with healthier testosterone levels and metabolic function.15
Additionally, gut health influences insulin sensitivity, which plays a key role in testosterone balance, particularly in conditions such as polycystic ovary syndrome (PCOS) and hypogonadism.
Comprehensive Testing for Root Causes
Utilizing the Gut Zoomer, Hormone Zoomer, and Salivary Hormones Panel offers a comprehensive perspective on hormonal imbalances.
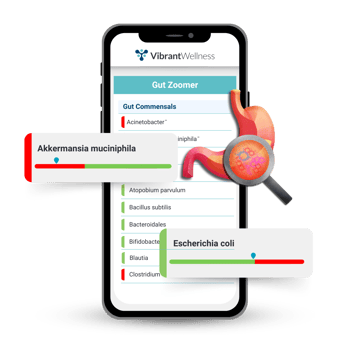 Gut Zoomer: Advanced Gut Microbiome Analysis
Gut Zoomer: Advanced Gut Microbiome Analysis
The Vibrant Wellness Gut Zoomer test provides a comprehensive analysis of the gut microbiome, identifying imbalances in bacteria, pathogens, and food sensitivities. It evaluates inflammation markers, SCFA levels, and dysbiosis, offering insights into how gut health impacts digestion, immunity, metabolism, and hormones.
With personalized recommendations for diet, probiotics, and lifestyle changes, the Gut Zoomer helps address chronic digestive issues, inflammation, and hormone-related conditions, providing actionable steps for improving overall health.
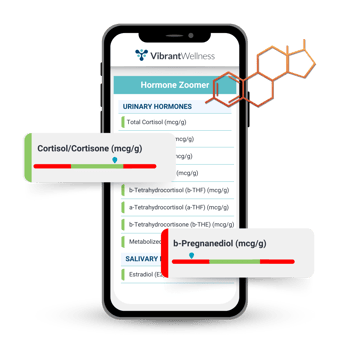 Hormone Zoomer: In-Depth Hormone and Metabolism Assessment
Hormone Zoomer: In-Depth Hormone and Metabolism Assessment
The Vibrant Wellness Hormone Zoomer test delivers a full-spectrum analysis of hormone balance, metabolism, and detoxification pathways. It measures sex hormones, adrenal hormones, and endocrine disruptors, providing a precise assessment of how hormones are processed and eliminated in the body.
By evaluating key hormone metabolites, this test helps identify imbalances that contribute to conditions such as estrogen dominance, adrenal fatigue, thyroid dysfunction, and metabolic disorders. Additionally, the Hormone Zoomer detects exposure to endocrine-disrupting chemicals like BPA and phthalates, offering critical insights into environmental influences on hormone health. With this information, providers can create personalized treatment plans that support hormone balance, detoxification, and long-term metabolic health.
Salivary Hormone Panel: Real-Time Adrenal and Stress Response Testing
The Vibrant Wellness Salivary Hormone Panel provides a dynamic, real-time assessment of cortisol, cortisone, and melatonin levels throughout the day. By tracking diurnal hormone patterns, this test helps evaluate adrenal function, stress responses, and circadian rhythm disruptions. It identifies abnormal cortisol fluctuations that may indicate adrenal insufficiency, HPA axis dysfunction, or chronic stress-related imbalances. Additionally, melatonin levels offer insights into sleep disturbances and overall endocrine regulation.
adrenal function, stress responses, and circadian rhythm disruptions. It identifies abnormal cortisol fluctuations that may indicate adrenal insufficiency, HPA axis dysfunction, or chronic stress-related imbalances. Additionally, melatonin levels offer insights into sleep disturbances and overall endocrine regulation.
With its ability to pinpoint adrenal dysregulation and stress-related hormone imbalances, the salivary hormone test supports targeted interventions such as adaptogenic therapy, stress management, and personalized lifestyle modifications to restore optimal hormonal function.
By combining these three tests, you can tailor interventions to address the root causes and support gut health and hormonal balance, rather than merely treating symptoms.
How Endocrine Disruptors Affect Menopausal Symptoms
Patient Profile
A 47-year-old female with chronic fatigue, low libido, weight gain, hot flashes and night sweats, vaginal dryness, headaches, and mood swings. The patient stated that she often woke up between 1:00 and 3:00 am and then struggled to fall back asleep. She was diagnosed with menopause at age 46.
Testing Insights
The Gut Zoomer revealed:
- Elevated inflammatory markers, including S100A12, sIgA, and beta-defensin 2
- Low percentages of butyrate and valerate short-chain fatty acids
- High levels of ß-glucuronidase and fecal zonulin
- Dysbiosis in lactobacilli, Prevotella, and Bifidobacterium species
- Low Akkermansia muciniphila levels
Salivary and urine hormone testing showed:
- Low testosterone
- Estrogen dominance
- Elevated cortisol
- Imbalanced estrogen metabolism
Interventions

After reviewing the test results, care providers recommended these interventions:
- Gut Support:
- Probiotics, including Saccharomyces boulardii, targeting both dysbiosis and inflammation reduction
- Fiber-rich diet and supplementation to support beneficial bacteria and promote estrogen metabolism
- A methylated B complex added to assist in estrogen metabolism
- A bitters complex added to assist in bile flow and detoxification of the liver and gallbladder
- Hormonal Balance:
- A methylated B complex added to assist in estrogen metabolism
- Bioidentical progesterone and estrogens started at low doses
- Zinc, DHEA, and vitamin D supplementation to support testosterone production
- A combination of holy basil, Relora, and l-theanine added to address cortisol imbalance
- Lifestyle Modifications:
- Strength training
- Intermittent fasting
- Stress reduction techniques, including box breathing and yoga
Outcome
After four months, the patient experienced increased energy, improved mood and sleep, and enhanced metabolic function leading to weight loss. Her vaginal vasomotor symptoms also improved.
Actionable Strategies for Providers
Supplement Support

Probiotics
Specific species of lactobaccili and bifidobacterium, along with Saccharomyces boulardii, can assist with managing dysbiosis.16 Probiotics can help restore balance in the microbiome and balance beta-glucuronidase activity, improving gut health and enhancing the gut barrier.16 They also help modulate the immune system and reduce inflammation.
Prebiotics
These food sources encourage beneficial gut bacteria growth, improving microbial balance. Prebiotics resist digestion in the upper gastrointestinal tract and reach the colon intact, where they are fermented by the gut microbiota.
This fermentation process produces short-chain fatty acids, which serve as energy sources for colonocytes and help maintain gut health. By promoting a favorable gut microbiota composition, prebiotics can enhance immune function, improve digestion, and potentially reduce the risk of certain diseases.17,18
Adaptogens
Adaptogens help regulate hormones and improve gastrointestinal health by modulating the body's stress response. Three key adaptogens include Ashwagandha (Withania somnifera), which reduces cortisol levels; Rhodiola rosea, known for balancing stress-related hormones; and Schisandra chinensis, which supports endocrine function.19
These adaptogens not only promote hormonal balance but also aid GI health, as stress significantly impacts digestion. By reducing stress-induced inflammation and supporting gut microbiota, adaptogens contribute to overall well-being.19
Hormone Replacement Therapy
Providing bioidentical hormone replacement therapy (BHRT) can assist patients who are struggling with andropause, PMS, perimenopause, and menopause. These individuals are often at a high risk for dysregulation due to a lack of hormones and impaired GI systems.
Hormones to monitor and consider replacement include estradiol, estriol, progesterone, DHEA, testosterone, and pregnenolone. Dosing is specific to the individual and should be tailored to reduce potential risks to patients, such as cancer.
There are many different ways to provide BHRT to your patients, such as oral, topical, sublingual, injectable, and pellet therapy. Each method comes with pros and cons to discuss with your patient prior to starting therapy.
Diet

A fiber-rich diet, such as whole grains, fruits, and vegetables, can help nourish beneficial gut bacteria, enhancing diversity and reducing inflammation. Fermented foods like yogurt, kimchi, and sauerkraut introduce probiotics, promoting a balanced gut environment.
These dietary habits help regulate estrogen metabolism and lower cortisol, the stress hormone, leading to improved hormonal balance. Cruciferous vegetables (broccoli, kale) and flaxseeds support liver detox pathways.20,21
Lifestyle Adjustments

Specific lifestyle practices can profoundly influence hormonal balance and overall health:
- Stress Reduction: Mindfulness practices, yoga, and deep breathing exercises help regulate cortisol production, promoting relaxation and reducing stress-related inflammation. These practices also enhance brain function and emotional resilience, contributing to overall well-being.22
- Exercise: High-intensity interval training (HIIT) and structured exercise training significantly influence hormonal regulation. HIIT enhances anabolic hormone secretion, including testosterone and growth hormone, which support muscle growth and metabolism. Additionally, exercise modulates cortisol levels, preventing excessive stress-related hormonal imbalances. Regular training improves insulin sensitivity, reducing the risk of metabolic disorders. By balancing stress and anabolic hormones, HIIT and exercise training promote overall endocrine health, improving energy regulation and physical performance.23
- Sleep Hygiene: Sleep plays a crucial role in regulating hormones and maintaining gut health. Inadequate sleep disrupts the balance of key hormones such as cortisol, insulin, ghrelin, and leptin, leading to increased stress, impaired metabolism, and appetite dysregulation. Poor sleep also negatively impacts the gut microbiota, contributing to inflammation and gastrointestinal issues. Prioritizing quality sleep supports hormonal balance, promotes digestive health, and reduces the risk of metabolic disorders, improving overall well-being.24
Establishing Gut Microbiome and Hormonal Balance
Understanding the gut-hormone connection is crucial for precision medicine. By utilizing Gut Zoomer and urinary and salivary functional hormone testing, you can uncover hidden imbalances in your patients' bodily systems and develop targeted interventions that lead to lasting improvements in hormonal health.
If you are seeking to optimize patient outcomes, Vibrant’s testing options offer an invaluable toolset. Implementing microbiome-based approaches can revolutionize patient care, leading to better hormonal balance, enhanced well-being, and improved quality of life.
About the Author
Dr. Logan Morse, PharmD, ABAAHP, FAAFRM, FACA, is an accomplished pharmacist and co-owner at Keystone Compounding Pharmacy in Grand Rapids, Michigan. He holds a Doctorate in Pharmacy from Ferris State University and is board-certified in anti-aging and functional medicine through the American Academy of Anti-Aging Medicine. Dr. Morse specializes in integrative and functional medicine. He works closely with patients on personalized health strategies, particularly in hormone replacement therapy, adrenal health, chronic fatigue, and sports medicine. Dr. Morse also serves in the United States Air National Guard, demonstrating his commitment to both his profession and his community. He is a passionate advocate for patient-centered care and is known for his deep dedication to helping patients achieve better health outcomes. Through tailored treatment plans and education on new treatment options, he aims to provide customized solutions tailored to improve patient outcomes.
References:
- Kwa M, Plottel CS, Blaser MJ, Adams S. The Intestinal Microbiome and Estrogen Receptor-Positive Female Breast Cancer. J Natl Cancer Inst. 2016;108(8):djw029. Published 2016 Apr 22. doi:10.1093/jnci/djw029
- Goedert JJ, Jones G, Hua X, et al. Investigation of the association between the fecal microbiota and breast cancer in postmenopausal women: a population-based case-control pilot study. J Natl Cancer Inst. 2015;107(8):djv147. Published 2015 Jun 1. doi:10.1093/jnci/djv147
- He S, Li H, Yu Z, et al. The Gut Microbiome and Sex Hormone-Related Diseases. Front Microbiol. 2021;12:711137. Published 2021 Sep 28. doi:10.3389/fmicb.2021.711137
- Lephart, E.D., Naftolin, F. Estrogen Action and Gut Microbiome Metabolism in Dermal Health. Dermatol Ther (Heidelb) 12, 1535–1550 (2022). https://doi.org/10.1007/s13555-022-00759-1
- Rusch JA, Layden BT, Dugas LR. Signalling cognition: the gut microbiota and hypothalamic-pituitary-adrenal axis. Front Endocrinol (Lausanne). 2023;14:1130689. Published 2023 Jun 19. doi:10.3389/fendo.2023.1130689
- He S, Li H, Yu Z, et al. The Gut Microbiome and Sex Hormone-Related Diseases. Front Microbiol. 2021;12:711137. Published 2021 Sep 28. doi:10.3389/fmicb.2021.711137
- Rusch JA, Layden BT, Dugas LR. Signalling cognition: the gut microbiota and hypothalamic-pituitary-adrenal axis. J Clin Endocrinol Metab. 2025;110(2): 456-467.
- Bailey MT, et al. Exposure to a social stressor alters the structure of the intestinal microbiota: implications for stressor-induced immunomodulation. Brain Behav Immun. 2011;25(3):397-407. doi:10.1016/j.bbi.2010.10.023
- Nuriel-Ohayon M, Neuman H, Ziv O, et al. Progesterone Increases Bifidobacterium Relative Abundance during Late Pregnancy. Cell Rep. 2019;27(3):730-736.e3. doi:10.1016/j.celrep.2019.03.075
- Harvard Medical School. (2022, February 28). Gut bacteria produce hormone involved in postpartum depression. Harvard Medical School. https://hms.harvard.edu/news/gut-bacteria-produce-hormone-involved-postpartum-depression
- Pletzer B, Poppelaars ES, Klackl J, Jonas E. The gonadal response to social stress and its relationship to cortisol. Stress. 2021;24(6):866-875. doi:10.1080/10253890.2021.1891220
- Yoon K, Kim N. Roles of Sex Hormones and Gender in the Gut Microbiota. J Neurogastroenterol Motil. 2021;27(3):314-325. doi:10.5056/jnm20208
- He S, Li H, Yu Z, et al. The Gut Microbiome and Sex Hormone-Related Diseases. Front Microbiol. 2021;12:711137. Published 2021 Sep 28. doi:10.3389/fmicb.2021.711137
- Santos-Marcos JA, Mora-Ortiz M, Tena-Sempere M, Lopez-Miranda J, Camargo A. Interaction between gut microbiota and sex hormones and their relation to sexual dimorphism in metabolic diseases. Biol Sex Differ. 2023;14(1):4. Published 2023 Feb 7. doi:10.1186/s13293-023-00490-2
- Santos-Marcos, J.A., Mora-Ortiz, M., Tena-Sempere, M. et al. Interaction between gut microbiota and sex hormones and their relation to sexual dimorphism in metabolic diseases. Biol Sex Differ 14, 4 (2023). https://doi.org/10.1186/s13293-023-00490-2
- Walton GE, Swann JR, Gibson GR. (2013). Prebiotics. In: Rosenberg E, DeLong EF, Lory S, Stackebrandt E, Thompson F. (eds) The Prokaryotes. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-30144-5_88
- He S, Li H, Yu Z, et al. The Gut Microbiome and Sex Hormone-Related Diseases. Front Microbiol. 2021;12:711137. Published 2021 Sep 28. doi:10.3389/fmicb.2021.711137
- Tóth-Mészáros A, Garmaa G, Hegyi P, et al. The effect of adaptogenic plants on stress: A systematic review and meta-analysis. Journal of Functional Foods. 2023;108:105695. https://doi.org/10.1016/j.jff.2023.105695
- Portincasa P, Bonfrate L, Vacca M, et al. Gut Microbiota and Short Chain Fatty Acids: Implications in Glucose Homeostasis. Int J Mol Sci. 2022;23(3):1105. Published 2022 Jan 20. doi:10.3390/ijms23031105
- Kau, A. L., Ahern, P. P., Griffin, N. W., Goodman, A. L., & Gordon, J. I. (2011). Human nutrition, the gut microbiome, and the immune system. Nature, 474(7351), 327-336. https://doi.org/10.1038/nature10213
- Zhang P. Influence of Foods and Nutrition on the Gut Microbiome and Implications for Intestinal Health. Int J Mol Sci. 2022;23(17):9588. Published 2022 Aug 24. doi:10.3390/ijms23179588
- Cahn BR, Goodman MS, Peterson CT, Maturi R, Mills PJ. Yoga, Meditation and Mind-Body Health: Increased BDNF, Cortisol Awakening Response, and Altered Inflammatory Marker Expression after a 3-Month Yoga and Meditation Retreat. Frontiers in Human Neuroscience. 2017;11(315). doi:https://doi.org/10.3389/fnhum.2017.00315
- Mohammadi S, Monazzami A, Alavimilani S. Effects of eight-week high-intensity interval training on some metabolic, hormonal and cardiovascular indices in women with PCOS: a randomized controlled trail. BMC Sports Science, Medicine and Rehabilitation. 2023;15(1). https://doi.org/10.1186/s13102-023-00653-z
- Leproult, R., & Van Cauter, E. (2010). Role of sleep and sleep loss in hormonal release and metabolism. Endocrine development, 17, 11–21. https://doi.org/10.1159/000262524
Regulatory Statement:
The general wellness test intended uses relate to sustaining or offering general improvement to functions associated with a general state of health while making reference to diseases or conditions. This test has been laboratory developed and its performance characteristics determined by Vibrant America LLC and Vibrant Genomics, a CLIA-certified and CAP-accredited laboratory performing the test. The lab tests referenced have not been cleared or approved by the U.S. Food and Drug Administration (FDA). Although FDA does not currently clear or approve laboratory-developed tests in the U.S., certification of the laboratory is required under CLIA to ensure the quality and validity of the test.
.png?width=50&name=Headshot%20(1).png) By
By